WHAT IS SIBO?
Small Intestinal Bacterial Overgrowth (SIBO) has been shown to be a primary cause of chronic digestive symptoms, as well as the commonly diagnosed condition, IBS.1,2,3
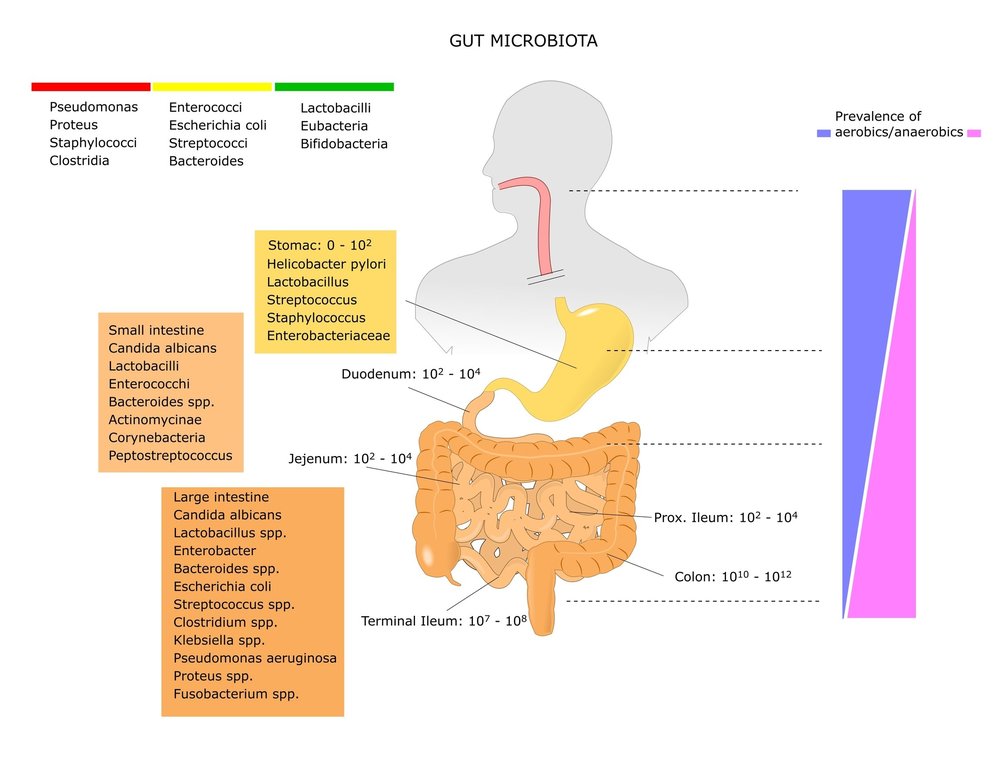
Why would this be? To begin understanding the connection, we must first understand the difference between the microbiome of the small intestines and the large intestine. Over 99% of our gastrointestinal bacterial communities should reside in our large intestine. Therefore, at most, there should only be 1% of our bacterial communities taking hold in our small intestines
The primary reason for this significant difference lies in the fact that gastrointestinal bacteria are fermenters of constituents found in our food. And therefore, significant producers of gas. Our small intestines have a very small diameter when compared to the large intestine. This smaller diameter allows for the efficient digestion of food and absorption of nutrients. However, this smaller space is not sufficient for excessive bacterial gas production.
Therefore, if we develop SIBO, there is now an excessive number of bacteria residing in the small intestines, which leads to an excessive amount of fermentation of constituents in our food, which ultimately leads to excessive bacterial gas production in our small intestines. This can lead to a significant expansion and ballooning out of the small intestines, which leads to direct gas-related symptoms, as well as symptoms one may not at first correlate with excessive gas production in the intestines.
Types of SIBO
There are 3 distinct forms of SIBO that can develop. A patient can have anywhere from 1 to all 3 types occurring. It is very common to have at least 2 forms occurring at the same time.
SIBO breath testing confirms exactly which form(s) your patient has developed.
The 3 types of SIBO are classified by the type of gas the bacteria produce. The 3 types are:
- Hydrogen (H2) producing SIBO
- Methane (CH4) producing SIBO
- Hydrogen Sulfide (H2S) producing SIBO
Mechanism of SIBO Symptoms
The primary constituents found in our food that gastrointestinal bacteria feed on, are:
- Fibres – specifically soluble fibre
- Sugars – specifically fructose and lactose
- Oligosaccharides
- Sugar alcohols
The above constituents are fed on and fermented by Hydrogen (H2) producing and Hydrogen Sulfide (H2S) producing bacteria. The single species of Methane (CH4) producing bacteria does not ferment and use these constituents as part of its metabolism. It has its own special fuel source listed below. Hydrogen Sulfide (H2S) bacteria shares one of these special fuel sources.
These extra fuel sources are:
- CO2 gas – used by CH4 producing bacteria
- H2 gas – used by CH4 and H2S producing bacteria
- Sulfur compounds – used by H2S producing bacteria
When the bacterial overgrowth feeds on and ferments any of the above constituents, they will produce a significant amount of their gas in the small intestines. This leads to the expansion of the small intestines and ultimately leads to the litany of SIBO symptoms.
SIBO symptoms can include:
- Excessive abdominal distension/bloating
- Excessive trapped gas and abdominal pressure
- Excessive flatulence (extremely pungent smelling in some cases)
- Excessive eructation
- Abdominal pains
- Halitosis
- GERD
- Nausea
- Diarrhea
- Constipation
It is clear to see why SIBO is an extremely common cause of chronic digestive symptoms, as well as the condition labeled as IBS.
Cause of SIBO
There is a clear and distinct connection between contracting a case of bacterial gastroenteritis (food poisoning/traveler’s diarrhea) and developing SIBO & IBS soon afterwards4,5,6. Depending on the study, anywhere between 1 in 5 to 1 in 9 people will develop SIBO/IBS after a case of bacterial gastroenteritis.
The piece that connects gastroenteritis and IBS, is SIBO. There is significant evidence that clearly shows how a case of food poisoning or traveler’s diarrhea leads to SIBO.
The migrating motor complex (MMC) is how we have been hard-wired to not develop SIBO from a very young age. Specifically, it is the Phase III of the MMC that triggers every 2.5 – 3 hours throughout the day, which ensures that bacteria do not pool in the small intestines. It is essentially the sweeping action of the small intestines, that forces bacteria to move from the small intestines into the large intestine but also inhibits bacteria from migrating in a retrograde fashion from the large intestine into the small intestines.
When the Phase III MMC system becomes damaged and weakened, the small intestinal contractions become too weak to prevent bacteria pooling in the small intestines, and SIBO develops.
How does bacterial gastroenteritis lead to long-term damage to the MMC function in many people? The answer is an autoimmune cross-reaction that unfortunately occurs in these patients post bacterial gastroenteritis infection. An antibody by the name of anti-vinculin is produced. When this occurs, the gastrointestinal immune system will target and damage components of one MMC for many months, leading to decreased MMC function, and ultimately SIBO/IBS develops7,8,9.
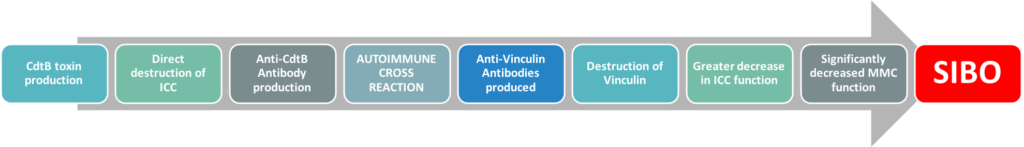
More information on this autoimmune cross reaction and how to test your patient for a history of it, please visit our IBS Smart page.
References:
- https://www.sciencedirect.com/science/article/abs/pii/S0002927000021614
- https://jamanetwork.com/journals/jama/article-abstract/199251
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3949258/
- https://pubmed.ncbi.nlm.nih.gov/28069350/
- https://bmcgastroenterol.biomedcentral.com/articles/10.1186/1471-230X-13-46
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4759150/
- https://pubmed.ncbi.nlm.nih.gov/12498278/
- https://link.springer.com/article/10.1007%2Fs10620-007-9977-z
- https://pubmed.ncbi.nlm.nih.gov/25424202/
